Karen Alderete Herrera, PharmD; Hennepin County
Background: Petek et al. explored the relationship between statin use and cognitive decline in individuals diagnosed with Alzheimer’s Disease (AD) and mixed dementia. The study aimed to look at the interaction between patient characteristics and medication features that may influence how statins affect cognitive function (Figure 1). The hypothesis posed by the authors suggests that statins' ability to penetrate the blood-brain barrier (BBB), influenced by factors like lipophilicity and molecular structure, connects to their impact on the risk of AD as measured by the mini-mental state examination (MMSE).
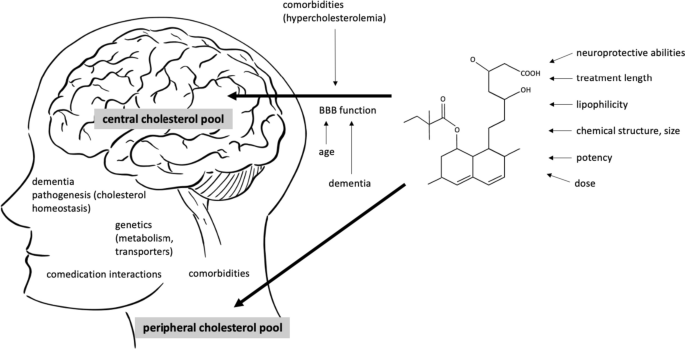
Figure 1 - The permeability of statins through the BBB is also influenced by aging, neurodegeneration, and peripheral hypercholesterolemia. The cognitive effects of statins likely stem from their actions in both the central and peripheral nervous systems.
Methods: The study utilized a longitudinal cohort approach by using the Swedish Registry for Cognitive/Dementia Disorders in combination with other national registries. Cognitive changes over time were assessed using the mini-mental state examination (MMSE), comparing scores between individuals who used statins and those who did not, as well as between different types of statins (statin type, dose, and duration) and non-statin lipid-lowering medications. Additionally, a dose-response analysis was conducted to compare cognitive outcomes between statin users and non-users.
Results: The study involved 15,586 patients with an average age of 79.5 years at diagnosis of AD, with a majority being women (59.2%). They found evidence of a dose-response effect: individuals who took one defined daily dose of statins, on average, exhibited an increase of 0.63 more MMSE points after 3 years compared to non-users (95% CI, 0.33 to 0.94) (Fig. 2). Furthermore, simvastatin users showed a greater increase of 1.01 MMSE points (95% CI, 0.06 to 1.97) compared to atorvastatin users after 3 years, particularly among younger individuals (<79.5 years at index date) (Fig. 3). Additionally, simvastatin users demonstrated a significant increase of 1.03 MMSE points (95% CI, 0.26 to 1.80) compared to rosuvastatin users after 3 years, with no observed differences regarding statin lipophilicity (Fig. 4). The authors noted that the sensitivity analysis focusing on incident users did not yield consistent results.
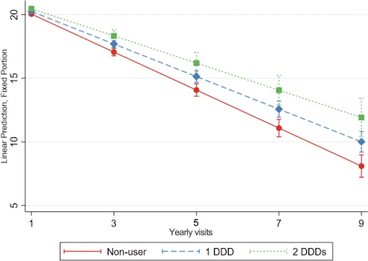
Figure 2
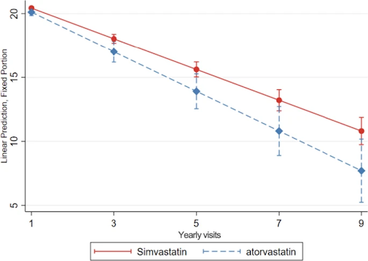
Figure 3
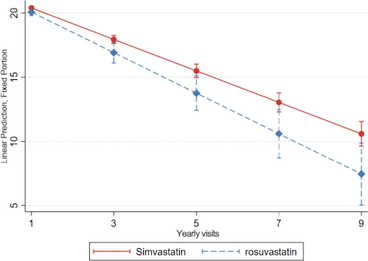
Figure 4
Conclusions: Overall, the study concluded that certain statins or longer durations of use may have greater benefits in preserving cognitive function in individuals with AD and mixed dementia. However, further research is needed to determine the specific mechanisms that could offer these effects to be then able to optimize statin therapy for cognitive preservation in AD and mixed dementia patients. While the overall association between statin use and slower cognitive decline was observed, the researchers found variations in effectiveness based on different factors which suggests that further research is needed.
Key Point: Patients with Alzheimer's Disease or mixed dementia and were on statins have shown to preserve cognitive function compared to patients not on statins. Although this effect is demonstrated in atorvastatin and rosuvastatin, the greatest effect was seen in simvastatin, seeing an increase of 1.03 points on the mini-mental state examination after 3 years of use. The current theory of statins preservation of cognitive function stems from their action in both central and peripheral nervous systems.
References:
- Petek, B., Häbel, H., Xu, H. et al. Statins and cognitive decline in patients with Alzheimer’s and mixed dementia: a longitudinal registry-based cohort study. Alz Res Therapy 15, 220 (December 2023).